Let me guess you stumbled across the word gastroshiza, paused for a second, and thought, “Okay, that sounds serious… but what is it actually?” Yeah, same here the first time I saw it. The term pops up all over blogs, parenting forums, and health sites, and it often leaves people confused, slightly alarmed, and reaching for Google at 2 a.m.
Here’s the deal: gastroshiza usually refers to gastroschisis, a real and medically recognized birth condition. The spelling may wander a bit online, but the topic stays the same. I’ve spent way too much time reading about it, comparing explanations, and trying to separate facts from internet noise. So let’s talk about it like normal humans, not like a medical textbook that forgot how conversations work.
Ready? Cool. Let’s break this down together.
Contents
- 1 What People Mean When They Say “Gastroshiza”
- 2 How Gastroshiza Develops During Pregnancy
- 3 How Doctors Detect Gastroshiza
- 4 Gastroshiza vs Omphalocele: Don’t Mix These Up
- 5 Treatment Options for Gastroshiza
- 6 Life in the NICU After Surgery
- 7 Long-Term Outlook: The Part Everyone Really Wants to Know
- 8 Emotional Side of a Gastroshiza Diagnosis
- 9 Why the Internet Makes Gastroshiza Sound Scarier Than It Is
- 10 Common Myths About Gastroshiza
- 11 How Doctors Continue Improving Outcomes
- 12 Why the Term “Gastroshiza” Keeps Circulating Online
- 13 What Parents Can Do After a Diagnosis
- 14 Final Thoughts: Why Gastroshiza Isn’t the End of the Story
What People Mean When They Say “Gastroshiza”
The Name Confusion (Yep, It’s a Thing)
First things first: “gastroshiza” isn’t an official medical term. Most experts and doctors use gastroschisis. Online writers and forums often swap spellings, which explains why you see both floating around.
Why does this matter? Because clarity saves stress. When parents search “gastroshiza,” they usually want answers about:
-
A birth condition
-
A visible abdominal issue in newborns
-
Treatment options and outcomes
And honestly, they deserve straight answers.
The Simple Explanation
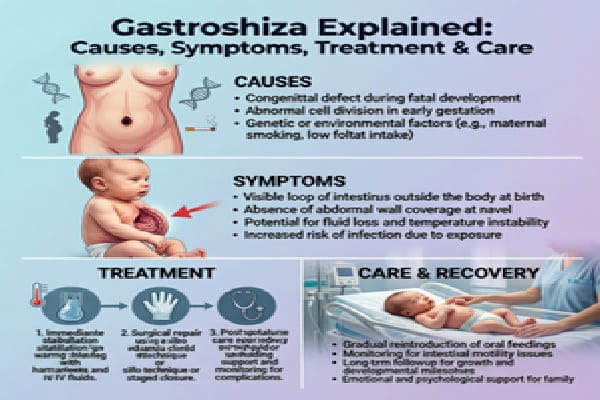
Gastroschisis is a birth defect where a baby is born with a hole in the abdominal wall, usually next to the belly button. Through that opening, parts of the intestines and sometimes other organs sit outside the body.
No cover. No protective sac. Just exposed organs that doctors need to handle carefully.
Sounds intense? Yeah. But medicine handles this better than you might think.
How Gastroshiza Develops During Pregnancy
What Goes Wrong (Development-Wise)
During early pregnancy, the baby’s abdominal wall forms and closes as organs settle into place. With gastroschisis, that closure doesn’t fully happen.
Doctors don’t blame parents for this, and they shouldn’t. This condition:
-
Happens very early in pregnancy
-
Occurs before most people even know they’re pregnant
-
Has no single confirmed cause
Ever wondered why the body sometimes misses a step? Biology can be messy like that.
Known Risk Factors (Not Causes)
Researchers link gastroschisis to a few patterns, but nothing guarantees it will happen:
-
Very young maternal age
-
Smoking or substance exposure during pregnancy
-
Certain environmental factors
FYI, plenty of parents with zero risk factors still have babies with gastroschisis. IMO, that unpredictability makes it scarier than it needs to be.
How Doctors Detect Gastroshiza
Prenatal Detection
Most cases show up during routine prenatal ultrasounds. Doctors spot intestines floating outside the baby’s body, which obviously raises flags.
Once doctors identify it, they:
-
Monitor growth more closely
-
Plan delivery at a specialized hospital
-
Coordinate with pediatric surgeons ahead of time
That planning makes a huge difference later.
At Birth: What It Looks Like
At delivery, gastroschisis becomes impossible to miss. The intestines sit outside the abdomen, usually to the right of the belly button.
This isn’t a “wait and see” situation. Medical teams act fast.
Gastroshiza vs Omphalocele: Don’t Mix These Up
People confuse these two conditions all the time. Let’s fix that.
Key Differences That Matter
Gastroschisis:
-
Organs sit outside the body
-
No protective sac
-
Smaller abdominal opening
-
Fewer genetic complications overall
Omphalocele:
-
Organs protrude through the belly button
-
Covered by a membrane
-
Often linked to chromosomal conditions
Why does this matter? Because gastroschisis often has a better long-term outlook, and parents deserve that reassurance.
Treatment Options for Gastroshiza
Surgery Comes First (Always)
Doctors treat gastroschisis with surgery shortly after birth. The goal stays simple:
-
Return the organs to the abdomen
-
Close the opening safely
-
Avoid pressure on the lungs or heart
Sounds straightforward, but execution takes skill.
Two Main Surgical Approaches
Primary Repair
-
Surgeons place organs back in one procedure
-
Works best when swelling stays minimal
-
Leads to quicker closure
Staged Repair
-
Doctors use a sterile pouch (called a silo)
-
Gradually move organs back over several days
-
Close the abdomen once swelling goes down
Surgeons choose based on the baby’s size, stability, and organ condition not convenience.
Life in the NICU After Surgery
The Recovery Phase
Babies with gastroschisis usually spend weeks in the NICU. That sounds terrifying, but it’s standard care.
During this time, doctors:
-
Support breathing if needed
-
Provide nutrition through IVs
-
Slowly introduce feeding once intestines wake up
Patience becomes the hardest part here. Trust me, waiting beats rushing.
Feeding Challenges (Temporary, Usually)
The intestines need time to recover. Some babies:
-
Tolerate milk quickly
-
Need weeks before feeding normally
Doctors monitor digestion closely. Once things move, everything else follows.
Long-Term Outlook: The Part Everyone Really Wants to Know
The Good News (Yes, There Is Plenty)
Here’s the honest truth: most babies with gastroschisis grow up healthy.
After recovery:
-
Growth often normalizes
-
Digestion improves
-
Development continues like any other child
Some kids face minor digestive sensitivity early on, but many outgrow it completely.
Possible Long-Term Issues (Not the Norm)
A small number experience:
-
Feeding intolerance
-
Bowel movement irregularities
-
Nutrient absorption challenges
Doctors catch these early and manage them well.
Ever notice how the internet loves worst-case scenarios? Reality usually looks calmer.
Emotional Side of a Gastroshiza Diagnosis
For Parents: It Hits Hard
Let’s not sugarcoat this. Hearing “your baby needs surgery at birth” rocks people.
Parents often feel:
-
Guilt (even when it’s not logical)
-
Fear of complications
-
Overwhelm from medical terms
I always say this: knowledge doesn’t erase fear, but it shrinks it.
Support Makes a Difference
Hospitals usually connect families with:
-
Neonatal specialists
-
Counselors or social workers
-
Other parents who’ve been there
No one handles this alone, even when it feels lonely.
Why the Internet Makes Gastroshiza Sound Scarier Than It Is
Clickbait vs Reality
Some articles frame gastroschisis like a tragedy headline. That approach helps clicks not families.
Reality looks more balanced:
-
Early detection improves outcomes
-
Surgery success rates stay high
-
Long-term quality of life remains strong
Scary words grab attention. Calm facts help people breathe.
The Power of Accurate Info
When parents understand:
-
What’s happening
-
Why doctors choose certain treatments
-
What recovery really involves
They regain control over the situation.
Knowledge equals steadiness. Always.
Also Read : Zuhagarten Explained: Smart, Simple, Modern Outdoor Living
Common Myths About Gastroshiza
Let’s clear the air.
-
Myth: Parents cause gastroschisis
Truth: No proven cause exists -
Myth: Babies won’t live normal lives
Truth: Most absolutely do -
Myth: Surgery always causes complications
Truth: Outcomes improve every year
Ever notice how myths thrive when facts hide? Yeah, let’s not let that happen here.
How Doctors Continue Improving Outcomes
Advancements That Matter
Medicine doesn’t sit still. Doctors now use:
-
Better surgical techniques
-
Improved infection control
-
Advanced nutritional support
Each improvement shortens hospital stays and improves comfort.
Prenatal Planning Saves Lives
When doctors diagnose gastroschisis early:
-
Teams prepare ahead of time
-
Deliveries happen at equipped hospitals
-
Surprises disappear
Preparation turns chaos into coordination.
Why the Term “Gastroshiza” Keeps Circulating Online
SEO, Misspellings, and Reality
People search what they hear. Writers repeat what people search. That loop keeps “gastroshiza” alive online.
But behind the spelling, the condition stays the same. Understanding that connection helps people land on accurate info faster.
And honestly? If spelling variations lead someone to real answers, I won’t complain 🙂
What Parents Can Do After a Diagnosis
Focus on What You Control
You can’t change the diagnosis, but you can:
-
Ask questions
-
Meet the surgical team early
-
Learn about the NICU process
Control reduces fear faster than anything else.
Prepare Emotionally, Not Perfectly
No one handles this perfectly. Some days feel strong. Others feel shaky.
Both count as progress.
Final Thoughts: Why Gastroshiza Isn’t the End of the Story
Let’s wrap this up honestly.
Gastroshiza better known as gastroschisis sounds terrifying at first glance. It involves surgery, hospital stays, and serious conversations. But it also involves skilled doctors, proven treatments, and resilient little humans who bounce back stronger than anyone expects.
If you’re here researching this topic, you’re already doing the right thing. You’re learning, preparing, and showing up.
And that? That matters more than any medical term ever will.